How to Heal Your Liver Fast: Treating Fatty Liver and NAFLD
In the past three months, I’ve on-boarded four patients who had been diagnosed with Non-Alcoholic Fatty Liver Disease (NAFLD), and, they were told by their doctor to “not worry about it.”
Well, let’s think about this…. an organ in your body has fat infiltration and we know that this will affect your liver’s ability to function and, if left unchecked, this can lead to more severe disease.
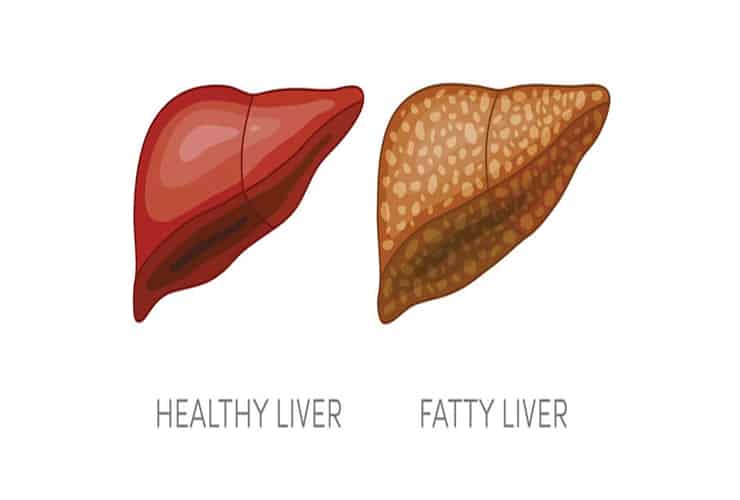
The old way of thinking, is that fatty liver is a symptom that’s being caused by another condition, or disease. The new way of thinking, is that fatty liver may be THE problem and it may be at the core of the problem (e.g. contributing to diabetes). Accumulating of fat in the liver is called steatorrhea of the liver.
The liver is the processing plant of the body – it processes toxins, creates nutrients, produces bile, activates enzymes, stores glucose, and it synthesizes proteins, among other things. It also makes cholesterol. So, your liver actually makes fat. When fatty liver is present, the liver is also storing fat (acting as a sponge). The number one driver of fatty liver is insulin resistance (which is often, but not always, driven by obesity).
Although the first thought with fatty liver is often that a person is eating too much fat and it’s the fat that’s causing fatty liver. Really, what’s happening here is that the carbohydrates (sugar) are triggering genes to turn on in the liver, which instructs the liver to convert sugar into fat.
A really good example of how this happens is to think of the process of creating Foie Gras (personally, I refuse to eat at a restaurant that serves this, as I believe that this is a truly barbaric practice). Geese are force-fed grains (not fats) to trigger fatty infiltration of the liver. Not only are they forced to eat too many calories, they are forced to consume grains as the source of the extra calories. Normal portioning of grains at meal times, along with a balanced caloric intake will not cause fatty liver in the average person. Yet, if excess calories from carbohydrates and sugar lead to excess weight and insulin resistance, we can see this pathway as a risk factor for fatty liver.
Diagnosing Fatty Live; NAFLD and NASH
There are a few markers on standard labs that indicate that the liver is stressed.
Standard testing:
- Liver function test and, or, comprehensive metabolic panel (CMP) is often the first pass of labs. If the two transaminases are even slightly elevated, Aspartate Transaminase (AST) and Alanine Transaminase (ALT), further investigation is warranted. AST and ALT are enzymes that are found only in the liver. When liver cells turn over they dump their contents, including AST and ALT. If the liver cells are turning over more rapidly (as happens when the liver is stressed) then AST and ALT will be found in higher concentrations in the blood.
- Alkaline Phosphatase is included in the CMP and if this is also elevated, it is a signal that the liver has been stressed longer term.
- Lipid Panel: elevated Triglycerides can lead to insulin sensitivity and diabetes. If triglycerides are elevated and HDL is low, then this is an indicator of metabolic syndrome and insulin resistance. Insulin resistance is a main cause of fatty liver.
Alternative test marker:
- Gamma-glutamyltransferase (GGT) – this is a more sensitive test, that isn’t often run on traditional labs. This is involved in glutathione metabolism. If this is elevated, this means that glutathione is being metabolized faster than usual, and this is telling us that the liver is under stress. GGT may be added to any standard test panel that is ordered.
If ALT and AST are elevated, then your practitioner will first determine if toxins or a virus are the cause. Toxins include excess alcohol, Tylenol, or other medications known to injure the liver. Once ‘drug induced liver injury’ (DILI) is ruled out, then you will be screened for viruses, like Epstein Barr. Once these are ruled out, the next step is to get an ultrasound to see if there is fatty infiltration of the liver.
NAFLD is diagnosed when more than 5% of your liver is replaced by fat. The ultrasound will not tell you the exact percentage of fatty liver infiltration. It will simply identify if you have more than 5% of fatty liver infiltration, and, if so, you will be diagnosed with fatty liver. If alcohol overuse is not the cause, if fatty liver infiltration is present without liver damage, the diagnosis will be NAFLD. The only way to confirm the amount of fatty liver infiltration, is through an invasive test that drives a needle from the outside of your body into your liver and biopsies the liver (this is usually not done).
Non-Alcoholic Fatty Liver Disease (NAFLD) is a diagnosis when simply a buildup of fat infiltration is present, without the presence of liver damage. The problem is, that in many cases, if NAFLD is left untreated over time, the immune system will become involved. When this happens, we can begin to see inflammation and damage to the liver. At this point NAFLD has now evolved into Non-Alcoholic Steatohepatitis (NASH). If NASH is left untreated, scarring can occur (called cirrhosis).
Also, to note, if you have fatty liver and your cardiac reactive protein (CRP) is elevated (>3), then this heightens your risk factors for further disease and complications from this.
Which Lifestyle Habits and Risk Factors Contribute to Fatty Liver?
- Obesity
- Hyperlipidemia
- Metabolic syndrome: large waist size, elevated triglycerides, low HDL, high blood pressure and high blood glucose
- Insulin Resistance
- Type 2 Diabetes
- Diet – processed sugar, high fructose corn syrup (HFCS), and excess grains/ calories, refined carbohydrates
- Inactivity, sedentary lifestyle
- Methylation issues (supplement with methylated folate)
The diet that has been studied and shown to be the most effective at helping to treat NAFLD is the Mediterranean Diet. This is not a carbohydrate free diet. It is a well portioned whole food carbohydrate diet (free of sugar, HFCS and refined carbohydrates).
Studies show that exercise lowers fat in the liver, regardless of weight loss. Exercise improves insulin resistance. Only 30 minutes of exercise five days a week has shown benefits. HIIT style workouts are more effective than steady state cardio.
The NAFLD Liver Treatment Protocol
I have taken the protocols that I’ve curated over 20 years in practice and shared them with our membership. You’ll find the exact brands and dosages in the FREE member section. Simply join for free (no hidden fees or membership upgrades, always free) AND enjoy a steep lifetime discount on all the professional lines we carry now and always!



